Eight FFR Measurements Using One TRUEPHYSIO® Pressure Microcatheter
By: Prof. Bernard De Bruyne & Dr. Jeroen Sonck

As interventional cardiologists are confronted with more complex patients, FFR measurement combined with multiple pullbacks is beneficial to guide PCI effectively and efficiently. The TruePhysio® pressure microcatheter can be easily delivered in challenging anatomies, while maintaining guidewire position throughout the pullback operation and assessments, and there is no need to rewire after stent implantation. This case highlights the essential need for TruePhsio microcatheter and multiple pullback assessments in a multivessel-disease scenario.
Patient History
57-year-old male
Asymptomatic and no angina
Lifestyle: Runs 10 triathlons annually
Risk factors: Hypertension
Primary PCI was performed on the distal left Circumflex (LCX) due to inferior-lateral STEMI on April 12, 2021
Case Challenges
Multivessel disease with several lesions in the proximal and the mid-to-distal LAD, in the D1 and in the posterolateral branch.
Multiple FFR measurements and pullback assessments are warranted in this complex procedure and a flexible pressure wire/microcatheter without losing the track will be extremely helpful.
Key learnings
This case highlights:
The need to have available microcatheter-based physiologic technology that allows the operator to get physiological insights into individual lesions in multiple vessels.
The role of pullback assessment in identifying the position of the culprit lesion.
In this case, FFR and pullback helped the operator optimize the PCI strategy and assess the improvement of function after revascularization in a short time.
RCA bifurcation lesion
TruePhysio® pressure microcatheter was delivered to the distal segment of the Posterior descending artery (PDA). After inducing hyperemia, FFR = 0.70
TruePhysio® pressure microcatheter was delivered to the distal posterolateral branch (PL) branch. After inducing hyperemia, FFR = 0.72
Functional ischemia induced by PDA/PL bifurcation lesion was identified, bifurcation stenting strategy was selected.
RCA was stented with a 2.5 mm × 30 mm DES optimizing with POT-side-POT
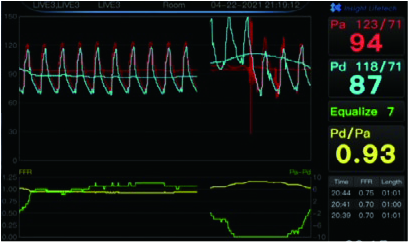
The post-PCI FFR measurement showed a value of 0.93 in the distal RCA (Fig. 1) and the recovery of blood flow (Fig. 2)
LAD and D1 Branch Lesion
FFR value of 0.65 was measured in the distal segment of the LAD, and a significant gradient showed in the most proximal segment of the LAD during pullback (Fig. 3)
FFR value was 0.73 in the distal D1
A gradient appeared when crossing the D1 lesion in the pullback process, while the bulk of the gradient was caused by the proximal of LAD (Fig. 4)
The proximal LAD and D1 needed to be treated with PCI, not the mid-to-distal LAD, the strategy changes a little bit compared with what physicians thought to do initially by angiograms.
D1 was stented with a 2.5 mm × 15 mm DES
Post-PCI FFR for D1 was 0.84, a gradient appeared in the D1 pullback process and it was assumed to be caused by proximal LAD (Fig. 5), and the stenosis in D1 was relieved (Fig. 6)
LAD was stented with a 3.0 mm × 23 mm DES and post dilatation was performed with a 3.5 mm × 15 mm NC balloon
Post-PCI FFR was 0.88 (Fig. 7) for the LAD and the recovery of blood flow in the proximal LAD (Fig. 8)
LCX Branch Lesion
With an FFR value of 0.96 in the distal LCX after hyperemia, the lesion was judged as non significant.
physician comments
It is impressive that we have performed 8 FFR measurements, including 8 pullbacks with the same microcatheter over the workhorse wire.
This allows performing multiple measurements during such complex procedures very flexibly.